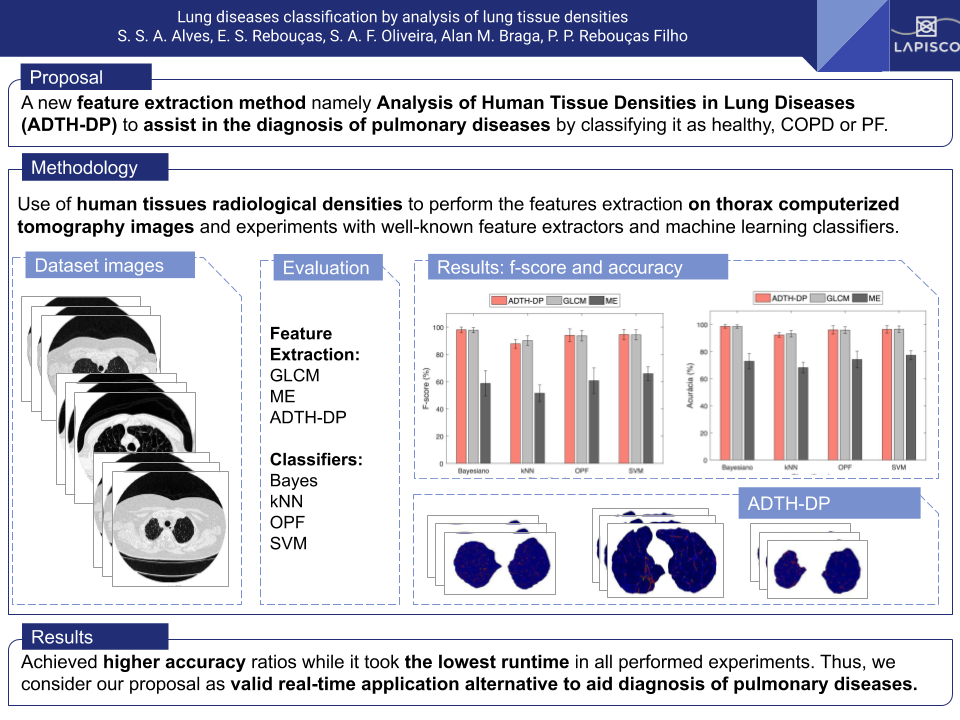
Lung Diseases Classification by Analysis of Lung Tissue Densities
Keywords:
Lung Disease, Lung, Computerized TomographyAbstract
Lung diseases identification based on analysis and processing of medical images is important to assist medical doctors during the diagnosis process. In this context, this paper proposes a new feature extraction method based on human tissue density patterns, namely Analysis of Human Tissue Densities in Lung Diseases. The proposed method uses human tissues radiological densities, in Hounsfield Units, to perform the features extraction on thorax computerized tomography images. We compared the proposed method against the Gray Level Co-occurrence Matrix and Statistical Moments to accomplish the performance evaluation alongside four machine learning classifiers. Overall, the results revealed that the proposal achieved higher accuracy ratios while it took the lowest runtime in all performed experiments. Thus, we consider our proposal as a valid alternative to be used in real-time applications.
Downloads
References
T. d. S. Cavalcante, P. Cortez, P. Rebouças Filho, J. Felix, A. Alexandria, and M. Holanda, “Comparative analysis of segmentation techniques of airways on images of chest computed tomography,” Signals and Image Processing, pp. 142–145, 2010.
P. P. Rebouças Filho, P. C. Cortez, and M. A. Holanda, “Active contour modes crisp: new technique for segmentation of the lungs in ct images,” Revista Brasileira de Engenharia Biomédica, vol. 27, no. 4, pp. 259–272, 2011.
P. P. Rebouças Filho, P. C. Cortez, J. H. da Silva Félix, T. da Silveira, and M. A. H. Cavalcante, “Modelo de contorno ativo crisp adaptativo 2d aplicado na segmentação dos pulmões em imagens de tc do tórax de voluntários sadios e pacientes com enfisema pulmonar,” Revista Brasileira de Engenharia Biomédica, vol. 29, no. 4, pp. 363–376, 2013.
J. H. S. Felix, P. C. Cortez, T. S. Cavalcante, A. R. Alexandria, P. P. Rebouças Filho, and M. A. Alcantara, Method of Automatic Initialization of Active Contours Applied to Lungs in Computed Tomography Images. Berlin, Heidelberg: Springer Berlin Heidelberg, 2013, pp. 1019–1022.
G. L. B. Ramalho, D. S. Ferreira, P. P. R. Filho, and F. N. S. de Medeiros, “Rotation-invariant feature extraction using a structural co-occurrence matrix,” Measurement, vol. 94, pp. 406 – 415, 2016. [Online]. Available: //www.sciencedirect.com/science/article/pii/S0263224116304730
E. C. Neto, P. C. Cortez, T. S. Cavalcante, V. E. Rodrigues, P. P. R. Filho, and M. A. Holanda, “3d lung fissure segmentation in tc images based in textures,” IEEE Latin America Transactions, vol. 14, no. 1, pp. 254–258, Jan 2016.
P. P. Rebouças Filho, P. C. Cortez, A. C. da Silva Barros, V. H. C. Albuquerque, and J. M. R. Tavares, “Novel and powerful 3d adaptive crisp active contour method applied in the segmentation of ct lung images,” Medical image analysis, vol. 35, pp. 503–516, 2017.
M. B. Rodrigues, L. B. Marinho, R. V. M. Nóbrega, J. W. M. Souza, and P. P. Rebouças Filho, Lung Segmentation in Chest Computerized Tomography Images Using the Border Following Algorithm. Cham: Springer International Publishing, 2017, pp. 539–548.
R. J. Mieloszyk, G. C. Verghese, K. Deitch, B. Cooney, A. Khalid, M. A. Mirre-Gonzalez, T. Heldt, and B. S. Krauss, “Automated quantitative analysis of capnogram shape for copd–normal and copd–chf classification,” IEEE Transactions on Biomedical Engineering, vol. 61, no. 12, pp. 2882–2890, 2014.
G. L. B. Ramalho, P. P. Rebouças Filho, F. N. S. d. Medeiros, and P. C. Cortez, “Lung disease detection using feature extraction and extreme learning machine,” Revista Brasileira de Engenharia Biomédica, vol. 30, no. 3, pp. 207–214, 2014.
G. Spina, P. Casale, P. S. Albert, J. Alison, J. Garcia-Aymerich, R. W. Costello, N. A. Hernandes, A. J. van Gestel, J. D. Leuppi, R. Mesquita et al., “Identifying physical activity profiles in copd patients using topic models,” IEEE journal of biomedical and health informatics, vol. 19, no. 5, pp. 1567–1576, 2015.
L. Nalysnyk, J. Cid-Ruzafa, P. Rotella, and D. Esser, “Incidence and prevalence of idiopathic pulmonary fibrosis: review of the literature,” European Respiratory Review, vol. 21, no. 126, pp. 355–361, 2012.
G. Raghu, S.-Y. Chen, W.-S. Yeh, B. Maroni, Q. Li, Y.-C. Lee, and H. R. Collard, “Idiopathic pulmonary fibrosis in {US} medicare beneficiaries aged 65 years and older: incidence, prevalence, and survival, 2001–11,” The Lancet Respiratory Medicine, vol. 2, no. 7, pp. 566 – 572, 2014. [Online]. Available: //www.sciencedirect.com/science/article/pii/S2213260014701018
E. C. O’Brien, M. T. Durheim, V. Gamerman, S. Garfinkel, K. J. Anstrom, S. M. Palmer, and C. S. Conoscenti, “Rationale for and design of the idiopathic pulmonary fibrosis–prospective outcomes (ipfpro) registry,” BMJ open respiratory research, vol. 3, no. 1, p. e000108, 2016.
J. Luis Lopez-Campos, W. Tan, and J. B. Soriano, “Global burden of COPD,” Respirology, vol. 21, no. 1, pp. 14–23, JAN 2016.
W. H. Organization, “Chronic obstructive pulmonary disease (copd),” http://who.int/mediacentre/factsheets/fs315/en/, nov 2016, accessed: 2017-01-31.
——, “The top 10 causes of death,” http://who.int/mediacentre/factsheets/fs310/en/, jan 2017, accessed: 2017-01-31.
M. N. et. al, “Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013,” Lancet, vol. 385, no. 9963, pp. 117–171, JAN 10 2015.
C. D. Mathers and D. Loncar, “Projections of global mortality and burden of disease from 2002 to 2030,” Plos Medicine, vol. 3, no. 11, NOV 2006.
R. de Marco, S. Accordini, I. Cerveri, A. Corsico, J. Sunyer, F. Neukirch, N. Kunzli, B. Leynaert, C. Janson, T. Gislason, P. Vermeire, C. Svanes, J. Anto, P. Burney, and E. C. R. H. Surve, “An international survey of chronic obstructive pulmonary disease in young adults according to GOLD stages,” Thorax, vol. 59, no. 2, pp. 120–125, FEB 1 2004.
A. Katzenstein and J. Myers, “Idiopathic pulmonary fibrosis - Clinical relevance of pathologic classification,” American Journal Of Respiratory And Critical Care Medicine, vol. 157, no. 4, pp. 1301–1315, APR 1998.
G. Raghu, H. R. Collard, J. J. Egan, F. J. Martinez, J. Behr, K. K. Brown, T. V. Colby, J.-F. Cordier, K. R. Flaherty, J. A. Lasky, D. A. Lynch, J. H. Ryu, J. J. Swigris, A. U. Wells, J. Ancochea, D. Bouros, C. Carvalho, U. Costabel, M. Ebina, D. M. Hansell, T. Johkoh, D. S. Kim, T. E. King, Jr., Y. Kondoh, J. Myers, N. L. Mueller, A. G. Nicholson, L. Richeldi, M. Selman, R. F. Dudden, B. S. Griss, S. L. Protzko, H. J. Schuenemann, and A. E. J. A. Comm, “An Official ATS/ERSARS/ALAT Statement: Idiopathic Pulmonary Fibrosis: Evidence-based Guidelines for Diagnosis and Management,” American Journal Of Respiratory And Critical Care Medicine, vol. 183, no. 6, pp. 788–824, MAR 15 2011.
E. S. White, Z. Borok, K. K. Brown, O. Eickelberg, A. Guenther, R. G. Jenkins, M. Kolb, F. J. Martinez, J. Roman, P. Sime, and A. T. S. R. Cell, “An American Thoracic Society Official Research Statement: Future Directions in Lung Fibrosis Research,” American Journal Of Respiratory And Critical Care Medicine, vol. 193, no. 7, pp. 792–800, APR 1 2016.
R. Prasad, N. Gupta, A. Singh, and P. Gupta, “Diagnosis of idiopathic pulmonary fibrosis: current issues,” Intractable & rare diseases research, vol. 4, no. 2, pp. 65–69, 2015.
T. E. King, Jr., A. Pardo, and M. Selman, “Idiopathic pulmonary fibrosis,” Lancet, vol. 378, no. 9807, pp. 1949–1961, DEC 3 2011.
K. Raimundo, E. Chang, M. S. Broder, K. Alexander, J. Zazzali, and J. J. Swigris, “Clinical and economic burden of idiopathic pulmonary fibrosis: a retrospective cohort study,” Bmc Pulmonary Medicine, vol. 16, JAN 5 2016.
P. Spagnolo, “Pirfenidone and mortality in idiopathic pulmonary fibrosis,” Lancet Respiratory Medicine, vol. 5, no. 1, pp. 3–5, JAN 2017.
J. H. da Silva Felix, P. C. Cortez, M. A. Holanda, and R. C. S. Costa, Automatic Segmentation and Measurement of the Lungs in healthy persons and in patients with Chronic Obstructive Pulmonary Disease in CT Images", bookTitle="IV Latin American Congress on Biomedical Engineering 2007, Bioengineering Solutions for Latin America Health: September 24th–28th, 2007 Margarita Island, Venezuela. Berlin, Heidelberg: Springer Berlin Heidelberg, 2008, pp. 370–373.
T. K. Liang, T. Tanaka, H. Nakamura, T. Shirahata, and H. Sugiura, “An Automated 3D Emphysema Extraction Method using Lung CT,” in 2008 Proceedings Of Sice Annual Conference, Vols 1-7, 2008, pp. 2994–2998, Annual Conference of the SICE, Chofu, JAPAN, AUG 20-22, 2008.
J. H. d. S. Felix, P. C. Cortez, and M. A. Holanda, “Sistema automático para quantificação e visualização da aeração pulmonar em imagens de tomografia computadorizada de tórax: Sistema de análise de imagens pulmonares: Saip,” Revista Brasileira de Engenharia Biomédica, vol. 26, no. 3, pp. 195–208, 2010.
T. da Silveira Cavalcante, P. C. Cortez, T. M. de Almeida, J. H. da Silva, and M. A. H. Felix, “Segmentação automática 2d de vias aéreas em imagens de tomografia computadorizada do tórax,” Revista Brasileira de Engenharia Biomédica, vol. 29, no. 4, pp. 389–403, 2013.
G. T. Herman, Fundamentals of computerized tomography: image reconstruction from projections. Springer Science & Business Media, 2009.
M.-K. Hu, “Visual pattern recognition by moment invariants,” IRE transactions on information theory, vol. 8, no. 2, pp. 179–187, 1962.
R. M. Haralick, K. Shanmugam et al., “Textural features for image classification,” IEEE Transactions on systems, man, and cybernetics, vol. 3, no. 6, pp. 610–621, 1973.
R. C. Gonzalez and R. E. Woods, Digital Image Processing (3rd Edition). Upper Saddle River, NJ, USA: Prentice-Hall, Inc., 2006.
M. Anthimopoulos, S. Christodoulidis, A. Christe, and S. Mougiakakou, “Classification of Interstitial Lung Disease Patterns Using Local DCT Features and Random Forest,” in 2014 36th Annual International Conference Of the IEEE-Engineering-in-Medicine-and-Biology-Society (EMBC), ser. IEEE Engineering in Medicine and Biology Society Conference Proceedings, 2014, pp. 6040–6043.
J. P. Papa, A. X. Falcao, and C. T. N. Suzuki, “Supervised Pattern Classification Based on Optimum-Path Forest,” International Journal Of Imaging Systems And Technology, vol. 19, no. 2, SI, pp. 120–131, 2009, 12th International Workshop on Combinatorial Image Analysis, Buffalo, NY, APR 07-09, 2008.
M. Anthimopoulos, S. Christodoulidis, L. Ebner, A. Christe, and S. Mougiakakou, “Lung Pattern Classification for Interstitial Lung Diseases Using a Deep Convolutional Neural Network,” Ieee Transactions On Medical Imaging, vol. 35, no. 5, SI, pp. 1207–1216, MAY 2016.
W. Zhao, R. Xu, Y. Hirano, R. Tachibana, and S. Kido, “Classification of Diffuse Lung Diseases Patterns by a Sparse Representation Based Method on HRCT Images,” in 2013 35th Annual International Conference Of the IEEE-Engineering-in-Medicine-and-Biology-Society (EMBC), ser. IEEE Engineering in Medicine and Biology Society Conference Proceedings, 2013, pp. 5457–5460.
A. A. A. Setio, A. Traverso, T. de Bel, M. S. Berens, C. v. d. Bogaard, P. Cerello, H. Chen, Q. Dou, M. E. Fantacci, B. Geurts et al., “Validation, comparison, and combination of algorithms for automatic detection of pulmonary nodules in computed tomography images: the luna16 challenge,” arXiv preprint arXiv:1612.08012, 2016.
N. Tajbakhsh and K. Suzuki, “Comparing two classes of end-to-end machine-learning models in lung nodule detection and classification: MTANNs vs. CNNs,” Pattern Recognition, vol. 63, pp. 476–486, MAR 2017.