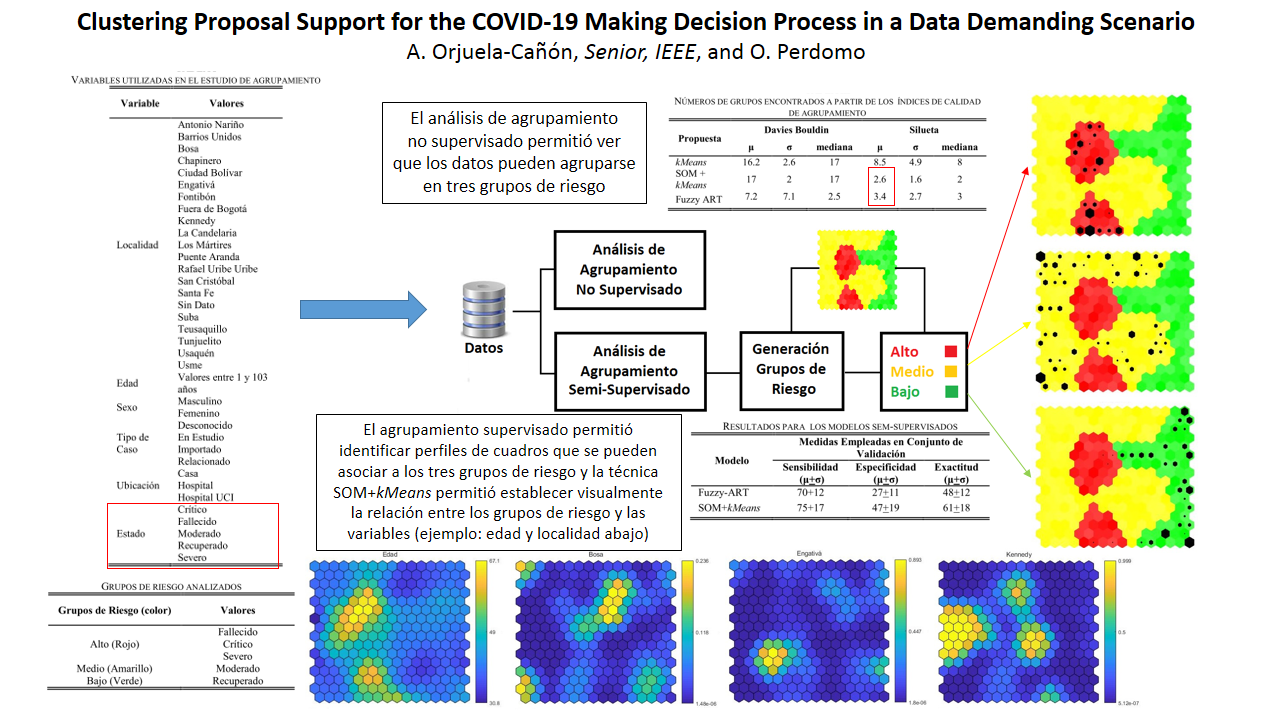
Clustering Proposal Support for the COVID-19 Making Decision Process in a Data Demanding Scenario
Keywords:
Artificial Intelligence, Clustering, Artificial Neural Networks, Decision Support Systems, COVID-19Abstract
The COVID-19 disease surprised the world in the last months due to the number of infections and deaths have been increased in an exponential way. Since the pandemic was established by the World Health Organization, different strategies have been proposed for dealing diverse problems in cities that the coronavirus affected. This work presents a method to decision making support processes, specifically in environment with few data and variables to be considered. Thus, artificial neural networks architectures were employed to cluster the information available in the Bogota city, and provide a tool that allows generating additional findings in a simultaneous mode, and expressed as a visual map. The present proposal reached sensitivity measures around 75%, obtaining 100% for the best cases.
Downloads
References
W. H. Organization and others, “WHO statement regarding cluster of pneumonia cases in Wuhan, China,” Beijing WHO, vol. 9, 2020.
N. Chen et al., “Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study,” Lancet, vol. 395, no. 10223, pp. 507–513, 2020.
A. Patel, D. B. Jernigan, and others, “Initial public health response and interim clinical guidance for the 2019 novel coronavirus outbreak--United States, December 31, 2019--February 4, 2020,” Morb. Mortal. Wkly. Rep., vol. 69, no. 5, p. 140, 2020.
E. S. C. de Coordinación de Alertas y, “Informe Técnico - Enfermedad por coronavirus, COVID-19,” 2020.
Y. Wang, M. Hu, Q. Li, X.-P. Zhang, G. Zhai, and N. Yao, “Abnormal respiratory patterns classifier may contribute to large-scale screening of people infected with COVID-19 in an accurate and unobtrusive manner,” arXiv Prepr. arXiv2002.05534, 2020.
B. N. Silva, M. Khan, and K. Han, “Towards sustainable smart cities: A review of trends, architectures, components, and open challenges in smart cities,” Sustain. Cities Soc., vol. 38, pp. 697–713, 2018.
M. I. Pramanik, R. Y. K. Lau, H. Demirkan, and M. A. K. Azad, “Smart health: Big data enabled health paradigm within smart cities,” Expert Syst. Appl., vol. 87, pp. 370–383, 2017.
Y. Wang et al., “Clinical information extraction applications: a literature review,” J. Biomed. Inform., vol. 77, pp. 34–49, 2018.
C. Xiao, E. Choi, and J. Sun, “Opportunities and challenges in developing deep learning models using electronic health records data: a systematic review,” J. Am. Med. Informatics Assoc., vol. 25, no. 10, pp. 1419–1428, 2018.
A. Manya and P. Nielsen, “Reporting practices and data quality in health information systems in developing countries: an exploratory case study in Kenya,” J. Health Inform. Dev. Ctries., vol. 10, no. 1, 2016.
Y. Glèlè Ahanhanzo, E.-M. Ouendo, A. Kpozèhouen, A. Levêque, M. Makoutodé, and M. Dramaix-Wilmet, “Data quality assessment in the routine health information system: an application of the lot quality assurance sampling in Benin,” Health Policy Plan., vol. 30, no. 7, pp. 837–843, 2015.
J. Macinko, F. C. Guanais, P. Mullachery, and G. Jimenez, “Gaps in primary care and health system performance in six Latin American and Caribbean countries,” Health Aff., vol. 35, no. 8, pp. 1513–1521, 2016.
N. Peek, C. Combi, R. Marin, and R. Bellazzi, “Thirty years of artificial intelligence in medicine (AIME) conferences: A review of research themes,” Artif. Intell. Med., vol. 65, no. 1, pp. 61–73, 2015.
F. Jiang et al., “Artificial intelligence in healthcare: past, present and future,” Stroke Vasc. Neurol., vol. 2, no. 4, pp. 230–243, 2017.
J. A. Hartigan, Clustering algorithms. 1975.
D. Xu and Y. Tian, “A comprehensive survey of clustering algorithms,” Ann. Data Sci., vol. 2, no. 2, pp. 165–193, 2015.
E. Elveren and N. Yumuvak, “Tuberculosis disease diagnosis using artificial neural network trained with genetic algorithm,” J. Med. Syst., vol. 35, no. 3, pp. 329–332, 2011.
P. Venkatesan and M. Mullai, “Clustering of Disease Data base using Self Organizing Maps and Logical Inferences,” Indian J. Autom. Artif. Intell., vol. 1, no. 1, pp. 2–6, 2013.
S.-L. Shieh and I.-E. Liao, “A new approach for data clustering and visualization using self-organizing maps,” Expert Syst. Appl., vol. 39, no. 15, pp. 11924–11933, 2012.
F. S. Aguiar, R. C. Torres, J. V. F. Pinto, A. L. Kritski, J. M. Seixas, and F. C. Q. Mello, “Development of two artificial neural network models to support the diagnosis of pulmonary tuberculosis in hospitalized patients in Rio de Janeiro, Brazil,” Med. Biol. Eng. Comput., vol. 54, no. 11, pp. 1751–1759, 2016.
G. A. Carpenter, S. Grossberg, and D. B. Rosen, “Fuzzy ART: Fast stable learning and categorization of analog patterns by an adaptive resonance system,” Neural networks, vol. 4, no. 6, pp. 759–771, 1991.
A. D. Orjuela-Cañón, J. E. C. Mendoza, C. E. A. García, and E. P. V. Vela, “Tuberculosis diagnosis support analysis for precarious health information systems,” Comput. Methods Programs Biomed., 2018.
A. D. Orjuela-Cañón and J. de Seixas, “Fuzzy-ART neural networks for triage in pleural tuberculosis,” in Health Care Exchanges (PAHCE), 2013 Pan American, 2013, pp. 1–4.
A. D. Orjuela-Cañón, J. M. de Seixas, and A. Trajman, “SOM Neural Networks as a Tool in Pleural Tuberculosis Diagnostic,” in Annals of the 11th Brazilian Congress on Computational Intelligence, 2013, pp. 1–5.
Alcaldía Mayor de Bogotá, “COVID-19 en Bogotá.” 2020.
Ministerio de Tecnologías de la Información y las Comunicaciones, “Guía para el uso y aprovechamiento de Datos Abiertos en Colombia.” 2016.
A. Agresti, An introduction to categorical data analysis, vol. 135. Wiley New York, 1996.
T. Kanungo, D. M. Mount, N. S. Netanyahu, C. D. Piatko, R. Silverman, and A. Y. Wu, “An efficient k-means clustering algorithm: Analysis and implementation,” IEEE Trans. Pattern Anal. Mach. Intell., vol. 24, no. 7, pp. 881–892, 2002.
S. Haykin, Neural Networks and Learning Machines, 3ra ed. Pearson, 2009.
C. Budayan, I. Dikmen, and M. T. Birgonul, “Comparing the performance of traditional cluster analysis, self-organizing maps and fuzzy C-means method for strategic grouping,” Expert Syst. Appl., vol. 36, no. 9, pp. 11772–11781, 2009.
J. Huang, M. Georgiopoulos, and G. L. Heileman, “Fuzzy ART properties,” Neural Networks, vol. 8, no. 2, pp. 203–213, 1995.
T. Kohonen, “Self-organizing maps, ser,” Inf. Sci. Berlin Springer, vol. 30, 2001. [33] M. Zribi, Y. Boujelbene, I. Abdelkafi, and R. Feki, “The self-organizing maps of Kohonen in the medical classification,” in Sciences of Electronics, Technologies of Information and Telecommunications (SETIT), 2012 6th International Conference on, 2012, pp. 852–856.
D. L. Davies and D. W. Bouldin, “A cluster separation measure,” IEEE Trans. Pattern Anal. Mach. Intell., no. 2, pp. 224–227, 1979.
P. J. Rousseeuw, “Silhouettes: a graphical aid to the interpretation and validation of cluster analysis,” J. Comput. Appl. Math., vol. 20, pp. 53–65, 1987.
L. Kaufman and P. J. Rousseeuw, Finding groups in data: an introduction to cluster analysis, vol. 344. John Wiley & Sons, 2009.
A. Ahmad and L. Dey, “A k-mean clustering algorithm for mixed numeric and categorical data,” Data Knowl. Eng., vol. 63, no. 2, pp. 503–527, 2007.
T.-H. T. Nguyen, D.-T. Dinh, S. Sriboonchitta, and V.-N. Huynh, “A method for k-means-like clustering of categorical data,” J. Ambient Intell. Humaniz. Comput., pp. 1–11, 2019.
S. Khanmohammadi, N. Adibeig, and S. Shanehbandy, “An improved overlapping k-means clustering method for medical applications,” Expert Syst. Appl., vol. 67, pp. 12–18, 2017.